Increasing access, equity and quality of emergency care by improving emergency nursing assessment
It’s not just during pandemics that nurses are on the frontlines of emergency care. The 300 emergency nurses of the Illawarra Shoalhaven local health district, New South Wales, Australia, provide care for more than 150,000 patients a year, a third of whom are children.
Nurses and other frontline emergency clinicians are responsible for the initial assessment, management and safety of critically ill patients. They are the first and sometimes the only clinicians that patients see, so the quality of their initial assessment and treatment is vital.
Emergency Care is a critical component for all healthcare systems and emergency presentations are increasing exponentially around the world. Improving emergency care saves lives, prevents secondary morbidity and reduces time to recovery. The timely recognition, treatment and management of the acutely ill at the appropriate levels of the health system is fundamental to the quality and safety of healthcare.
Emergency departments are a uniquely challenging healthcare environment. The role of emergency clinicians is starkly different from that of other specialties. They assess and initiate care with varying degrees of clinical urgency and severity for patients of all ages, most of whom are undiagnosed and undifferentiated.
Emergency clinicians, including nurses, perform a comprehensive assessment and, when needed, start investigations and interventions. This assessment underpins clinical decisions and safe care by preventing, detecting and acting upon deterioration. The quality and timeliness of this assessment is crucial as emergency patients often have extended waiting times for higher level review. Failure to recognise and respond to patients whose condition deteriorates increases the incidence of high-mortality adverse events.
Structured approaches to trauma patient assessment, such as the primary survey, improve care delivery and patient outcomes. Standardisation in generic emergency assessment beyond Airway, Breathing and Circulation improves the value of emergency assessment, reduces unwarranted variation in care, facilitates timely recognition and response to clinical deterioration, reduces time to definitive treatment, and maximises quality outcomes. Improved clinical assessment is recognised as an area of need by the World Health Organization.
“HIRAID” which stands for History, Identify Red flags, Assessment, Interventions, Diagnostics, communication and reassessment (Figure 1), is the only comprehensive assessment framework that can be applied to all patients in the emergency setting. Its application is not dependent on context, clinical skill level or resources. It was developed by Professor Kate Curtis and her team for optimal emergency care delivery.
Figure 1
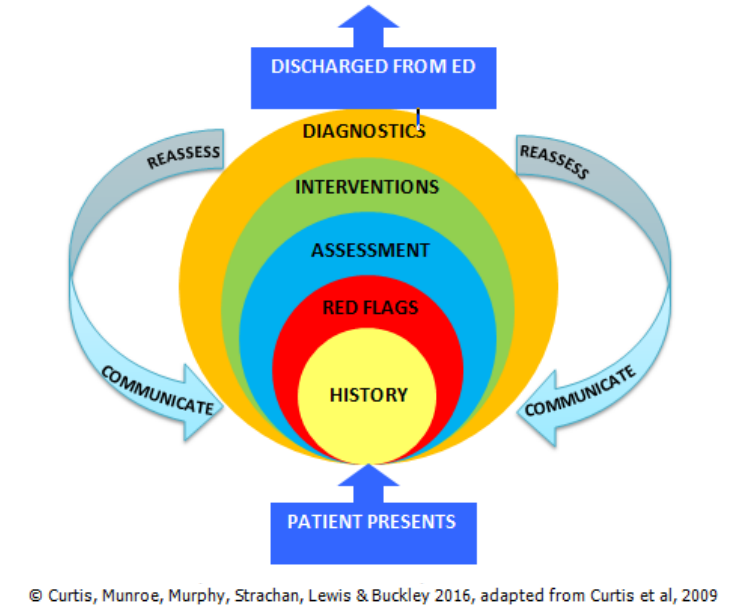 |
HISTORY: Collection of presenting problem and health history. |
| IDENTIFY RED FLAGS: Historical and physiological indicators of urgency to recognise potential and actual serious illness. Notify red flags to a senior ED medical officer as soon as possible. | |
| ASSESSMENT: Clinical examination should include: primary survey, focused head-to-toe examination, vital signs, inspection, auscultation, and palpation. | |
| INTERVENTIONS: Interventions should be evidence based and prioritised based on assessment. | |
| DIAGNOSTICS: Order investigations necessary to gain an overall clinical picture of the patient and inform treatment decisions. Perform and review in a timely manner
REASSESSMENT: The evaluation of care and monitoring of patient progress. Maintain a structured approach, repeat at appropriate intervals per condition of the patient. COMMUNICATION: Verbal/non-verbal communication skills necessary to effectively communicate with patients, families and clinicians. Use structured approach to clinical handover, graded assertiveness to escalate and comprehensive documentation. |
|
An implementation toolkit and education package for emergency nurses has been developed to include this new model, which is now used in clinical practice at multiple emergency departments in Australia and internationally.
The resources available for implementation of HIRAID include published literature demonstrating the evidence base for the components of HIRAID and the effectiveness of HIRAID when applied; curriculum/lesson plans/facilitator manual for early career nurses and ‘train the trainer’ practical group training; teaching resources; and an implementation tool kit informed by behaviour change techniques.
Using HIRAID, emergency nurses improve their self-efficacy, communication and detection of clinical and historical indicators of urgency. All these essential aspects of clinical nursing practice contribute to improved patient care and outcomes. Emergency nursing and medical staff perceived HIRAID to be a useful tool for use in the clinical environment to improve consistency, documentation and communication.
In keeping with the Sustainable Development Goals (SDGs), attending to human emergencies with timely, optimal medical care meets Goal 3, that of Good Health and Well-Being. HIRAID ‘train the trainer’ workshops have been held in Nepal, Sri Lanka, Fiji, Colombia and around Australia.

